Transient Ischemic Attack (TIA)
A transient ischemic attack, or TIA, is a temporary blockage of blood flow to the brain. The clot usually dissolves on its own or gets dislodged, and the symptoms usually last less than five minutes.
While a TIA doesn’t cause permanent damage, it’s a “warning stroke” signaling a possible full-blown stroke ahead. When you first notice symptoms, get help immediately, even if symptoms go away.
Risk Factors and TIA
Anyone can have a TIA, but the risk increases with age. Stroke rates double every 10 years after age 55. If you’ve previously had a stroke, pay careful attention for signs of a TIA because that could signal a second stroke in your future.
Common warning signals include sudden onset of:
- Weakness, numbness or paralysis on one side of your body
- Slurred speech or difficulty understanding others
- Blindness in one or both eyes
- Dizziness
- Severe headache with no apparent cause
Major risk factors for a TIA or stroke include:
High blood pressure
Diabetes
Heart disease
Atrial fibrillation
Smoking
Diagnosis and Treatment
TIAs’ temporary symptoms, which can last from only a few minutes up to 24 hours, make diagnosis challenging. Stroke symptoms that disappear in under an hour need emergency assessment to help prevent a full-blown stroke.
Get help immediately if you think you could be having a TIA. Ideally your comprehensive evaluation should be done within 24 hours of when symptoms began. Here is what you can expect:
- Assessment for symptoms and medical history
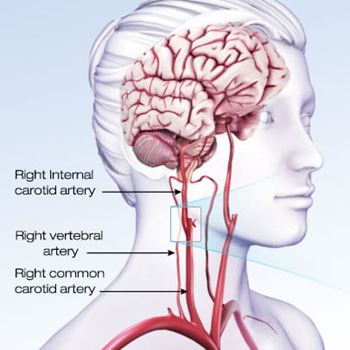
- Imaging of the blood vessels in the head and neck
- Other testing such as head CT, angiography and MRI
Once TIA is diagnosed, a follow-up visit with a neurologist is recommended to assess your risk of future stroke.
Some signs of TIAs are only visible with hospital equipment, so trained medical staff need to evaluate the patient’s condition. Appropriate medical care may include:
Assessing Vital Signs and Testing Brain Function
Initial assessment includes tests to help determine if cranial nerves are intact, vision is normal, muscles have strength and speaking and thinking seem normal. Heart rate, temperature and blood may also help provide an overall picture of what’s happening.
Imaging and Tests
Checking the blood flow and tissue within the brain tissue may be important to determine the cause of a TIA or any brief symptoms of stroke. A magnetic resonance imaging (MRI) scan or computerized tomography (CT) scan can show the images. An electrocardiogram (ECG) is often helpful. The main artery leading from the heart to the brain, called the carotid artery, may also be checked for signs of stiffening or blockage.
Medical History
Assessing medical history and cardiovascular disease risks, along with evaluating blood chemistry, can help determine the appropriate medication to prevent blood clots or a procedure to remove fatty deposits (plaques) from the arteries that supply blood to brain (carotid endarterectomy).
Referring a patient to a specialist is sometimes appropriate. When a TIA occurs with no clear risk factors for stroke, a neurologist may do test to rule out vasculitis, carotid artery dissection and other types of injury or infection.

Why Getting Quick Stroke Treatment is Important
Stroke symptoms, even if they disappear within an hour, need emergency assessment
Warning of Future Strokes



